Hernia Surgery
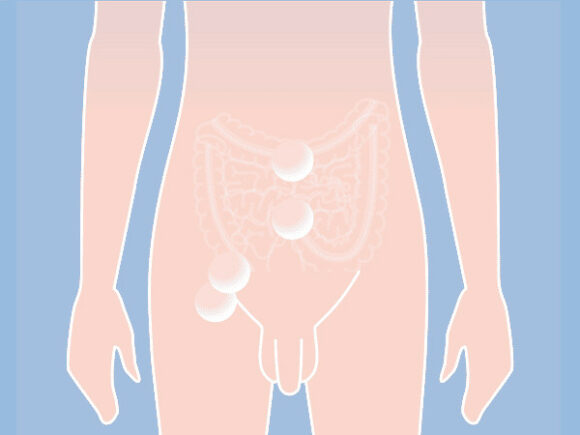
A hernia is a defect in the abdominal wall from which the contents of the abdomen protrude outwards from under the skin. Patients generally see a swelling and have discomfort or pain. Hernias are the most common surgical indication, and around 20,000 hernia operations are performed throughout Switzerland every year. The inguinal hernia is the most common, followed by hernia of the abdominal wall (e.g. umbilical hernias, scar hernias) flowed by rare causes such as flank hernia and diaphragmatic hernias.
At our centre for hernia surgery in Switzerland (Basel, Liestal, Zurichwe offer you competent and tailor-made advice and diagnostics:
- Inguinal Hernias
- Umbilical Hernias
- Diastasis recti
- Sportsman’s Groin
- Chronic postoperative inguinal pain
- Hiatal Hernia
Depending on the clinical picture and the individual requirements of our patients, we perform open (larger skin incision) and minimally invasive surgical techniques (keyhole surgery) in accordance with current scientific findings and guidelines. Our many years of surgical experience enable us to offer you a surgical technique tailored to your needs. For minimally invasive operations, in many cases we also use a latest-generation surgical robot (Intuitive da Vinci Xi) which uses a 3D image to allow us to use the instruments even more precisely and gently.
We perform our operations at our exclusive partner, Merian Iselin Clinic in Basel. This clinic located in the center of Basel is of high renown in north-west Switzerland. In addition, we have specialized in the treatment of sportsmen’s groin, chronic groin pain after hernia operations and rectus diastasis. These diseases are complex and must be treated together with other specialists and therapists. Here we can rely on a network of experienced sports physicians, physiotherapists, radiologists and pain therapists.
Our patients are also individually cared for and treated by us after the operation. We remain available for you at all times. Within the framework of our “quality-assured hernia surgery”, we also send out follow-up questionnaires after the operation in order to identify new problems early on and treat them professionally.